Digestive Health
By Dr Saravana K.


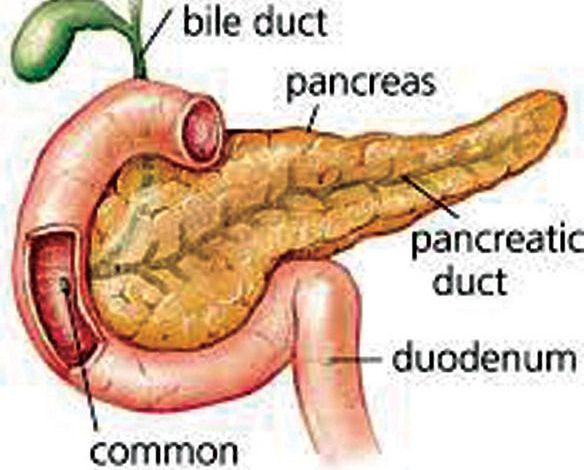
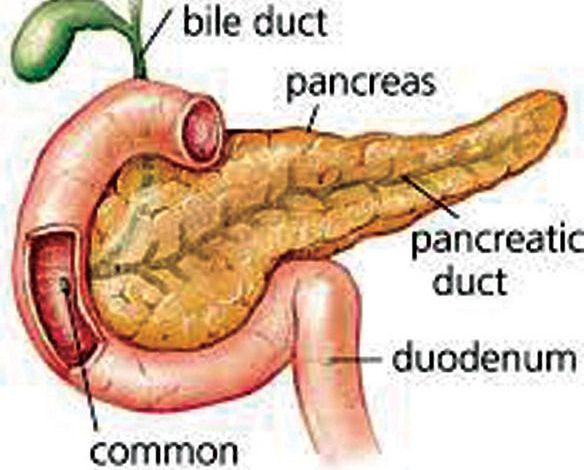
- Facilitate the digestion of carbohydrates, proteins and fat by secreting digestive enzymes into the small intestine.
- Release hormones, insulin and glucagon, into the bloodstream which are involved in blood glucose metabolism.
Pancreatitis is a rare disease in which the pancreas becomes inflamed. Damage occurs when the digestive enzymes are activated and begin attacking the pancreas. In very severe cases, pancreatitis can result in bleeding into the gland itself; serious tissue damage, infection and fluid collections may occur. Severe pancreatitis can result in damage to the heart, lung and kidneys. Long-standing inflammation in your pancreas caused by chronic pancreatitis is a risk factor for developing pancreatic cancer.
There are two forms of pancreatitis:
- Acute pancreatitis occurs suddenly and may result in life-threatening complications; however the majority of patients recover completely.
- Chronic pancreatitis is usually the result of longstanding damage to the pancreas.
Causes
Alcoholism; gallstones; abdominal surgery; medications; family history of pancreatitis; high calcium levels which may be caused by an overactive parathyroid gland; high triglyceride levels; infection; injury to the abdomen; or pancreatic cancer.
Symptoms
Most patients have upper abdominal pain that travels through the back. The abdomen may be swollen and very tender.
Symptoms of chronic pancreatitis include: pain; weight loss or diarrhoea; diabetes; nausea and vomiting; or fever.
The pain of chronic pancreatitis is usually constant in nature and radiates to the back. In some patients, this pain may be disabling. The weight loss is usually due to the patient’s inability to secrete pancreatic enzymes to break down food so nutrients are not absorbed normally. Finally, diabetes may develop if the insulin-producing cells in the pancreas are damaged.
Diagnosis
- Checking the blood for levels of digestive enzymes such as amylase.
- CT scan, MRI scan or abdominal ultrasound to look for gallstones and assess the extent of pancreas inflammation.
- Endoscopic ultrasound to look for inflammation and blockages in the pancreatic duct or bile duct.
Treatment
Acute pancreatitis is primarily treated with supportive management in the hospital. Generally, patients receive intravenous fluids and pain medication. In up to 20 per cent of patients, the pancreatitis can be severe. The patient may need to be placed in the intensive care unit because of damage that has occurred to other vital organs. Some cases of severe pancreatitis require surgery to remove irreversibly damaged parts of the gland. Once pancreatitis is brought under control, your health care team can treat the underlying cause of your pancreatitis.
Treatment will depend on the cause of your pancreatitis, but examples of treatment may include:
- Procedures to remove bile duct obstructions.
- Gallbladder surgery.
In chronic pancreatitis adequate pain relief, pancreatic enzymes and insulin to supplement what is not being secreted by the pancreas are given. In some instances, blockage of the pancreatic duct would require a surgical drainage procedure.
For more information call Saravana. K Gastroenterologist and Liver Specialist Clinic at Hospital Fatimah (05 548 7181) or email gastrosara@gmail.com.